For many individuals suffering from asthma and chronic obstructive pulmonary disease (COPD), Symbicort represents a life-enhancing medication. However, the relief it provides comes at a substantial financial cost. As a combination of budesonide, an anti-inflammatory corticosteroid, and formoterol, a long-acting beta-agonist, Symbicort is a critical maintenance therapy for many. Yet, despite its necessity, the price point remains exorbitant for a significant portion of the patient population, often necessitating harsh financial decisions for what is essentially an indispensable element of daily health management.
The steep pricing of Symbicort can be attributed to a variety of factors, including research and development costs, marketing, and the complex nature of inhaler production. Patients in the United States are acutely aware of the high price tag, which can run into hundreds of dollars for a single inhaler without the cushioning of insurance or discounts. Even with insurance, copays can be sizable, leaving many to wonder about the ethical implications of such a cost barrier to what should be routine, accessible healthcare for a common condition affecting millions.
Inhaler Economics: Why Symbicort Prices Skyrocket
Symbicort, a combination inhaler used to manage asthma and COPD, has seen a significant rise in price over the years, prompting questions about the factors that contribute to its escalating cost. The price surge can be attributed to a variety of factors, including research and development expenses, marketing costs, and the value of innovation in pharmaceuticals. The drug's effectiveness and the added convenience of having two medications in one inhaler justify the premium to some extent. However, the manufacturer's pricing strategies and the complexities of insurance and pharmacy benefit managers also play a substantial role in the final cost to consumers.
The lack of generic competition, owing to patent protections and FDA exclusivity, has allowed Symbicort's manufacturer to maintain high prices. This situation is exacerbated by the intricate and often non-transparent pharmaceutical pricing system in the United States, where drug prices are not regulated as they are in many other countries. Additionally, the costs associated with regulatory compliance and maintaining market exclusivity contribute to the high price point. These factors combine to create a financial burden for patients who rely on this medication for essential respiratory relief, spotlighting the need for more affordable alternatives.
Generic Vs. Brand-name: the Symbicort Price Divide
Symbicort, a branded medication containing a combination of budesonide and formoterol, is a standard treatment for asthma and COPD. Its efficacy in managing and preventing asthma symptoms comes with a high price tag, largely due to the costs associated with research and development, marketing, and the maintenance of safety standards. This price can be out of reach for many patients, particularly those without adequate insurance coverage, leading to a significant financial burden and potential compromise in treatment quality.
In contrast, generic medications are typically less expensive because they do not bear the same development and marketing costs as their brand-name counterparts. However, for a long time, the lack of a generic equivalent for Symbicort in many markets meant patients had little choice but to pay the premium for breathing. The introduction of generic versions has begun to alleviate some financial strain, yet the cost disparity between generic and brand-name Symbicort continues to be a pressing issue for many patients seeking accessible asthma and COPD treatments.
The Breath of Monopoly: Patent Laws and Symbicort
Patent protections have long been a double-edged sword in the pharmaceutical industry, fostering innovation while simultaneously constraining market competition. Symbicort, a popular asthma and COPD medication, is no exception. Its patent, which AstraZeneca has successfully defended, allows it to exclusively sell the drug, preventing generic competitors from entering the market. This exclusivity, while rewarding the company's investment in research and development, also means that the price of Symbicort can be kept at a premium without pressure from lower-cost alternatives, posing a significant financial barrier for many patients.
As the debate around drug patents continues, the Symbicort situation serves as a case study of the complexities involved. While patents are intended to last for a limited time, pharmaceutical companies often employ strategies to extend their monopolies, such as making slight modifications to the original formula or engaging in pay-for-delay tactics with potential generic competitors. These practices have drawn criticism from various stakeholders, including healthcare professionals and patient advocacy groups, who argue that they contribute to the persistent high costs of medications like Symbicort, which are critical for patients' health and well-being.
The Hidden Toll: Symbicort's Impact on Healthcare Systems
Symbicort's steep price point extends its impact beyond the individual patient level, influencing the broader terrain of healthcare economics. It is not simply a matter of direct costs for those requiring the medication, but the ripple effects are felt across healthcare systems that must allocate significant funds for this essential treatment. High expenditure on branded medications such as Symbicort can drain resources, leading to budget constraints that may affect the quality and availability of other services. Insurance companies, as well, may pass on the cost to consumers through higher premiums, while underfunded public healthcare systems may be forced to limit accessibility to life-saving drugs.
This financial strain can lead to difficult choices, both for healthcare providers and patients. On one hand, healthcare systems may restrict the use of Symbicort to the most severe cases or negotiate strenuously for price reductions, which can be a complex and challenging process. On the other hand, patients, especially those uninsured or underinsured, might skip doses, seek out international pharmacies, or forgo treatment altogether, potentially leading to more severe health complications and increased long-term costs. The high price of Symbicort thus not only burdens individual finances but also strains the collective purse of healthcare systems, underscoring the need for a sustainable solution to medication pricing.
Seeking Alternatives: Strategies for Affordable Breathing Solutions
As the cost of Symbicort and similar prescription medications continue to impose a financial burden on patients, individuals and healthcare providers alike are propelled to seek out more budget-friendly alternatives for managing respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). One of the primary strategies involves turning to generic medications, which contain the same active ingredients and provide comparable therapeutic effects at a fraction of the cost. Moreover, patient assistance programs offered by pharmaceutical companies, non-profits, or government agencies can provide significant relief by offering discounts or even free medications to those who qualify.
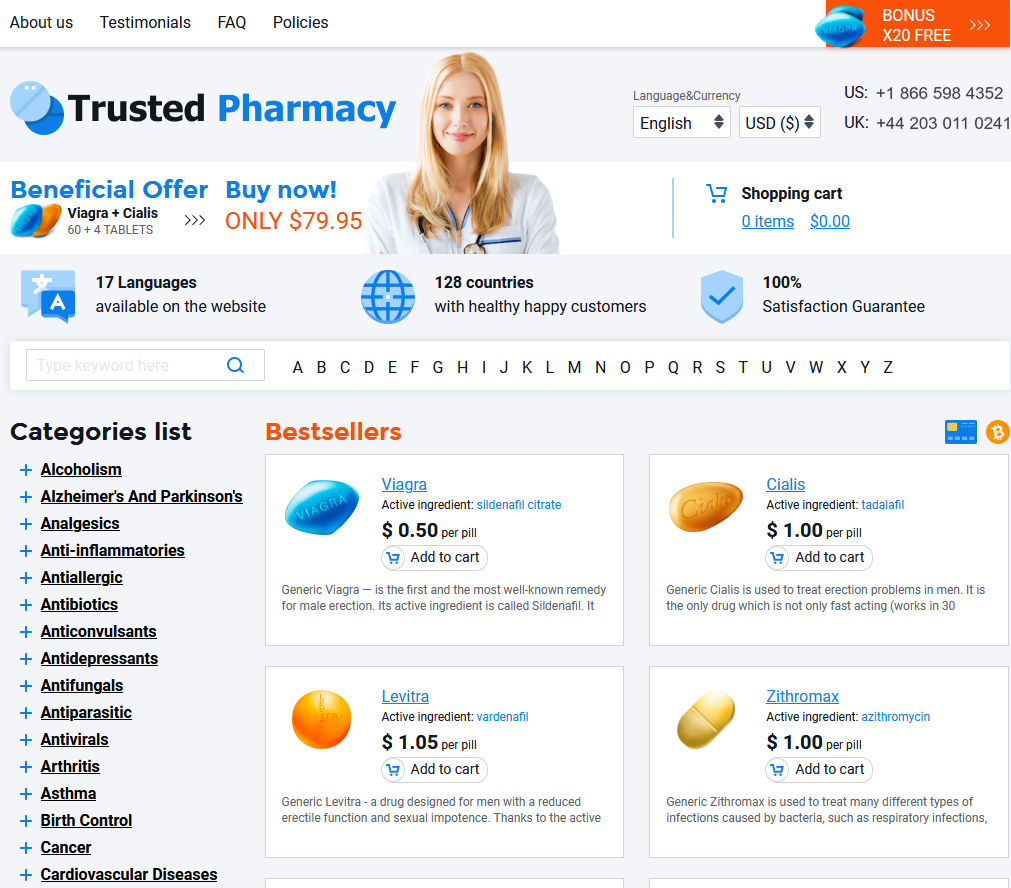
Another avenue worth exploring is the use of international pharmacies, which may offer Symbicort at lower prices due to different cost structures in other countries. Coupled with this, doctors might suggest therapeutic alternatives that are less expensive but still effective. Beyond pharmacological solutions, lifestyle modifications, such as smoking cessation, regular exercise, and breathing exercises, can also improve lung function and decrease the dependence on costly medications. Ultimately, the concerted efforts of policy change advocates, who are pushing for more competitive drug pricing and patent reforms, aim to reshape the pharmaceutical landscape to prioritize patient access and affordability over monopolistic profit margins.
Elavil Rybelsus Rifadin